Search for network providers
|
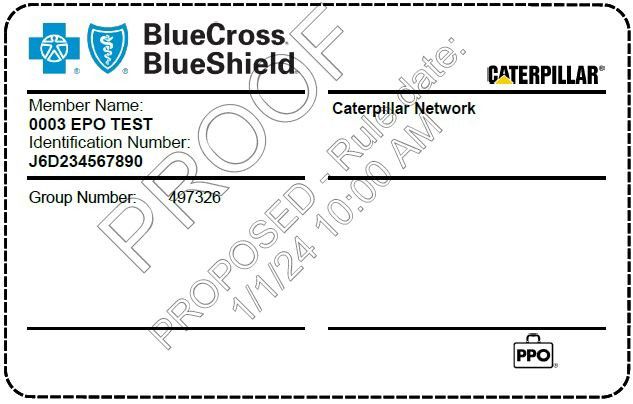
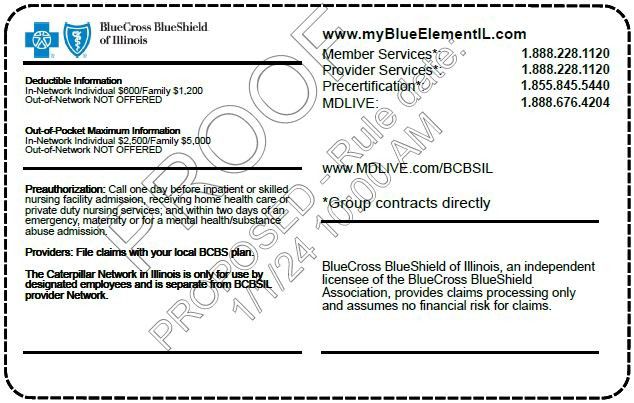
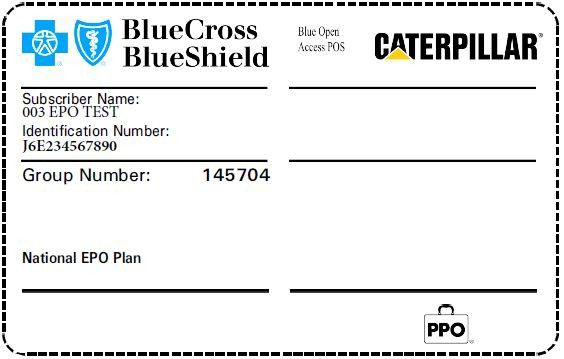
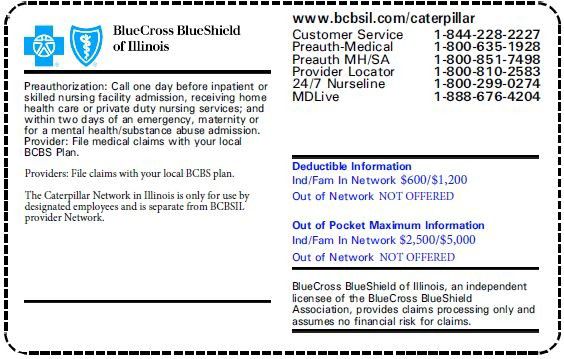
BCBS National |
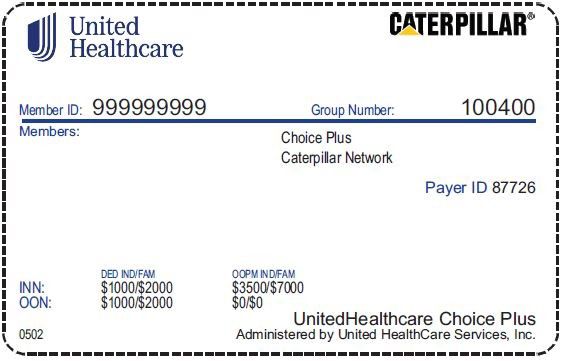
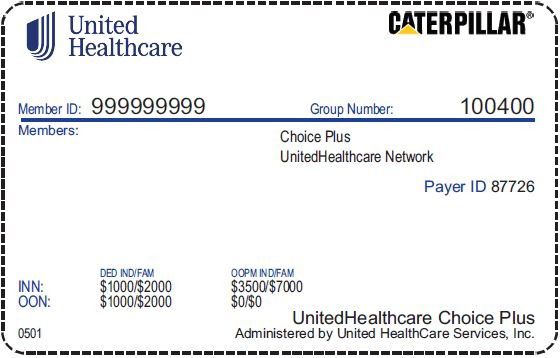
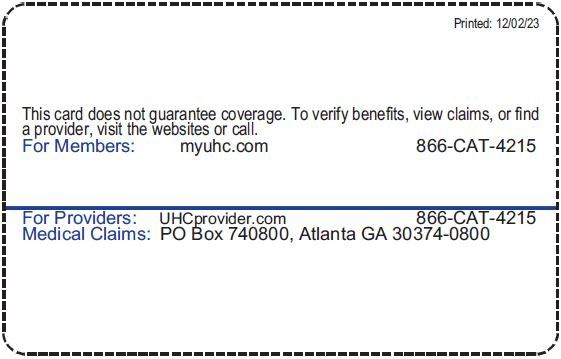
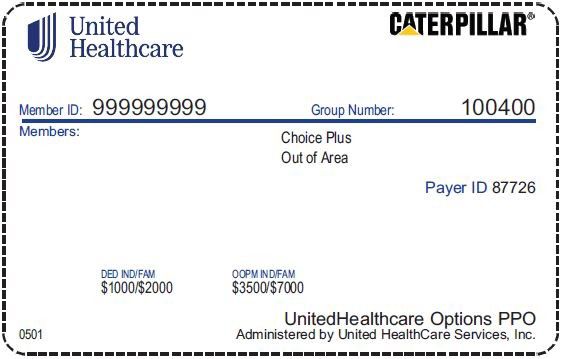
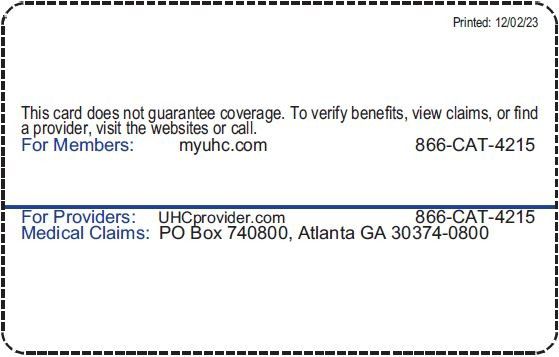
UHC Choice Plus, UHC Consumer Choice or UHC Consumer Max |
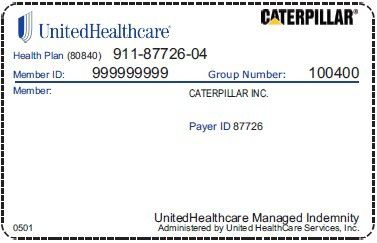
Out-of-Area Plan |
Indemnity Plan |
Network |
Blue Cross Blue Shield network
|
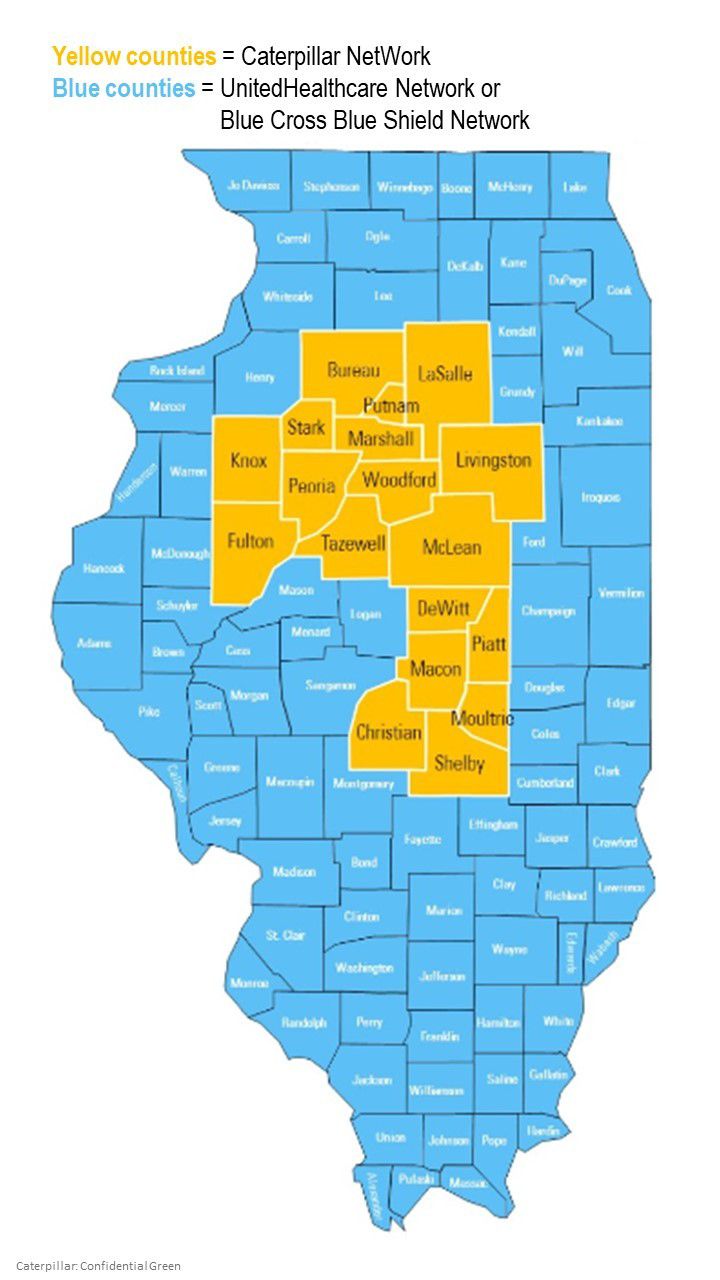
Either the: Caterpillar NetWork (if you live within one of the yellow counties on this this map) or UHC Choice Plus network (if you live outside of the yellow counties on this map) |
No network required, however, you may have UHC Choice Plus providers in your area |
No network required |
Provider Search |
Search for Caterpillar NetWork providers Search for UHC Choice Plus providers (select the Choice Plus option) Traveling out of the NetWork or need out-of-network services? |
Search for UHC Choice Plus providers (select the Choice Plus option) |
N/A |